Our Story and Mission



What Users Say
Hear from our empowered community.
Fasting Planet transformed my health and sleep routines completely!
The guidance on this site is invaluable for beginners like me.
Blog
Top 10 Signs You Might Have Sleep Apnea and Don’t Know It
Sleep apnea is more common than most people realize — yet many go years without…
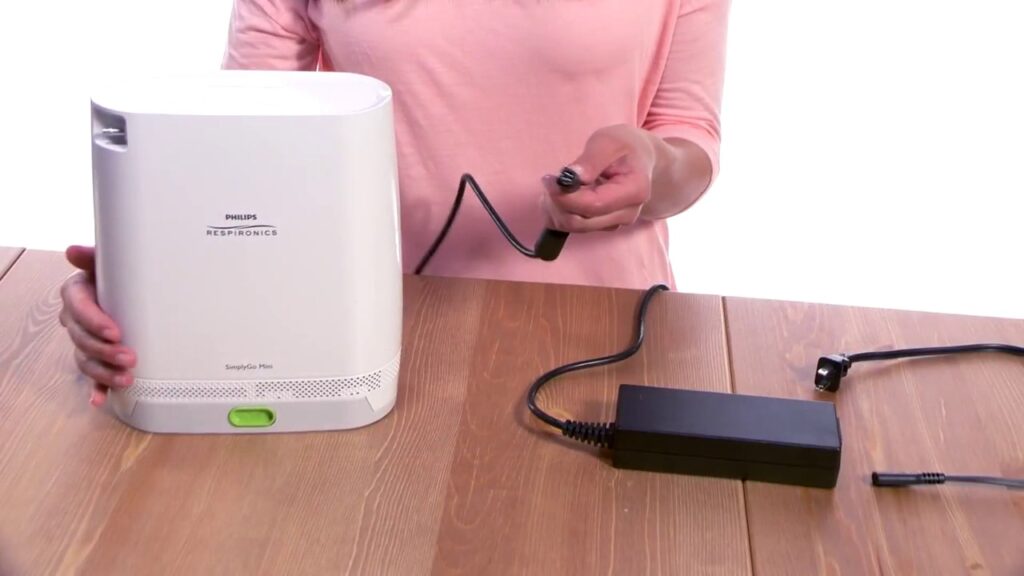
What Is a Portable Oxygen Concentrator and How Does It Work?
What Is a Portable Oxygen Concentrator? A portable oxygen concentrator (POC) is a compact, lightweight…
How Long Does a Portable Oxygen Cylinder Last on One Charge?
Portable oxygen cylinders typically last around 4 hours on a single charge or fill, though…
Sleep Study Hobart: What to Expect from Local Testing Services
Sleep disorders affect millions of Australians, silently undermining their health, productivity, and quality of life….
Canberra Sleep Study Cost: What You’ll Pay and Why
What is a Sleep Study and Why is it Important for Diagnosing Sleep Disorders Like…
NDIS Occupational Therapy in Castle Hill: What Families Need to Know
Occupational therapy (OT) plays a crucial role in the lives of individuals with disabilities, particularly…
Our Journey
Visual stories of health and wellness.